Unit 1.2
Strategies for Developing Systems Thinking
NLN Competency: II
Objectives
- Learner will be able to describe systems thinking
- Learner will be able to discuss why it is important to teach systems thinking to nursing
students - Learner will be able to name specific strategies for developing systems thinking in nursing
students
Introduction
Today’s healthcare environment is often very complex, involving an entire health care system, numerous stakeholders, many kinds of team members, and advanced processes and technology. In order to safely and efficiently care for patients and effectively solve complicated health care problems, nurses need to understand the relationships between all the parts of the health care system in which they work (examples of parts of a system may include people, products, processes, services, and regulations), the interactions between those parts, and the results of those interactions. That process of understanding how everything works together and affects each other is referred to as systems thinking (Bacon et al., 2018).
Importance of Teaching Systems Thinking
As health care becomes more complex, nursing education does not always prepare students very well for the challenges they face as new graduate nurses. For example, nursing students are often taught concepts and skills without discussing how to apply those same concepts and skills in a multidisciplinary team setting where many factors from all the interconnected parts of the healthcare system must be considered. Because of that lack of knowledge, employers often find that new graduate nurses do not know how to delegate tasks, struggle to handle multiple responsibilities and difficult problems, and not take the initiative because they do not understand the system (Clark & Hoffman, 2019). Teaching nursing students systems thinking can help them overcome those challenges and many others by expanding their view from just themselves and their individual actions to themselves within a greater system; the effect their actions have on the system, and the effect the system, in turn, has on their actions. When they have learned that, they can interact more smoothly with the different parts of the systems and begin to understand how to bring about change within that system (Clark & Hoffman, 2019). A key characteristic of systems thinking is that one must be able to anticipate the impact of one’s actions on the whole and then realize how actions can positively influence outcomes for the greatest good. An essential ability of systems thinking is to cognitively shift back and forth from the patient to the organization. Two common examples often used to explain cognitive shifting are:
1. Seeing the big picture; and
2. Taking a bird’s eye view of a situation.
Experienced nurses can foster this ability among students.
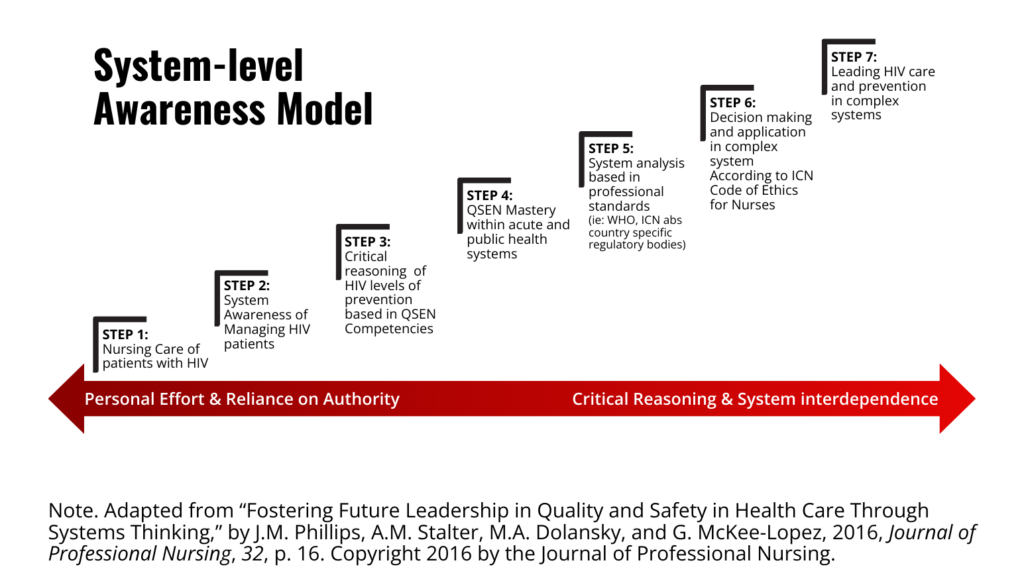
Teaching Systems Thinking Using the System-level Awareness Model
One way of teaching systems thinking that can be incorporated into nursing curricula is the System-level Awareness Model, also referred to as SAM. Using SAM, a novice nurse or nursing student who is not thinking in terms of systems advances through seven successive steps of systems thinking growth until step seven is reached – a professional nurse with a strong knowledge of systems thinking, who is prepared to lead in a complex health care environment. The seven steps build on each other, meaning a student or new nurse cannot successfully reach the next step without understanding and demonstrating the attitudes, skills, and behaviors of the steps below it. Because of the progressive nature of this model, it can be introduced into the curriculum at the start of a nursing program and then used throughout the program in beginner, intermediate, and advanced classroom, clinical, and simulation environments (Phillips & Slater, 2016). SAM incorporates the Quality and Safety Education for Nurses (QSEN) competencies in steps three and four because systems thinking plays a critical role in the successful adoption and application of the QSEN competencies (Phillips et al., 2016; Dolansky & Moore, 2013). As students progress, they reduce the amount of personal effort they put into systems thinking, become less reliant on authority figures, increase critical reasoning, and increase their awareness of interdependence. The SAM is presented below as adapted for HIV education. However, it can be used for any nursing concepts of interest or patient problems.
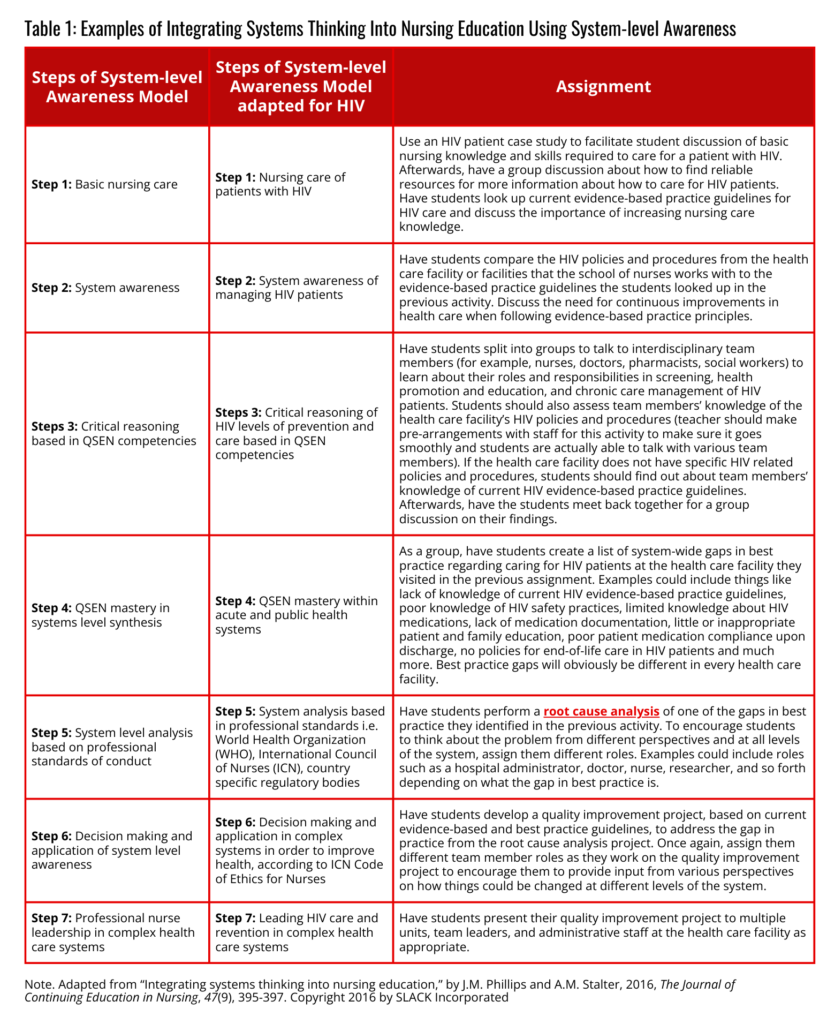
System-level Awareness Model Adapted for HIV Education
The following table provides an example of how the SAM can be used to integrate systems thinking during a class. In this example, the single topic of human immunodeficiency virus (HIV) offers one assignment per step. However different topics could be used throughout each step and for each assignment. Furthermore, many different assignments could be created that would work to teach the different steps of the model.
Further Strategies for Teaching Systems Thinking to Nursing Students (Clark & Hoffman, 2019)
- Add content to the nursing curriculum that introduces students to systems thinking concepts.
- Teach students to use TeamSTEPPS to give them the skills needed to work collaboratively with an interdisciplinary team.
- Require interprofessional education by creating a class applicable to students from multiple health care disciplines that is a general requirement (for example, an introduction to health care systems class for all medical, nursing, pharmacy, physical therapy, and health care administration students). Having students from multiple areas of the healthcare system taking a class together builds their understanding of interprofessional teams, exposes them to learning about scopes of practice, and teaches them communication, collaboration, and teamwork skills essential to systems thinking.
- Peer-to-peer learning groups where groups are made up of students from multiple health care and healthcare-related disciplines. This helps students make connections between different parts of the system and learn more about/learn to respect each other’s areas of practice.
- Teach students to use whatever kinds of technology they will be working on within the health care systems they will be working on. For example, if students will be using electronic medical records in the health care system they will be entering, they should be taught how to navigate electronic medical records. To fully understand systems thinking, students need to understand how technology works within the healthcare system.
- Use simulation. Simulation helps students better understand relationships between processes in realistic, complex decision-making scenarios.
Conclusion
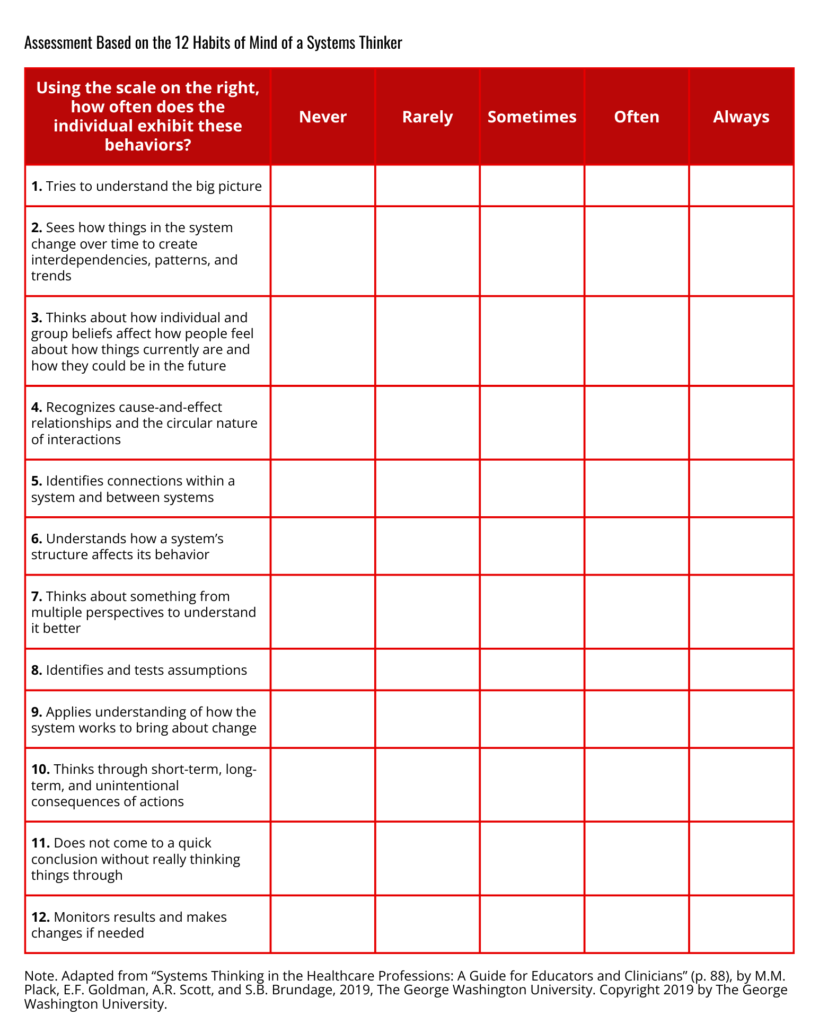
In today’s complex health care environment, it is extremely important for nurses to understand systems thinking. When new graduate nurses enter the workforce without knowledge of systems thinking, they are not fully prepared to be safe and effective team members or leaders. As such, systems thinking should be taught in nursing school and can be integrated into nursing curricula via the System-level Awareness Model. Nursing educators can evaluate the progression of systems thinking in students by having them complete the Systems Thinking Scale, a validated
tool for assessing the effectiveness of education to increase systems thinking (Dolansky et al., 2020) at the beginning and end of the nursing program and/or assess student activities and behaviors throughout the program using the 12 “habits of mind” of a systems thinker assessment tool (Plack et al., 2019) provided below.
Resources
- Dolansky and Moore’s Systems Thinking Scale
- Materials for teaching QSEN competencies to students
- Systems Thinking in the Healthcare Professions: A Guide for Educators and Clinicians by faculty at The George Washington University
- TeamSTEPPS learning materials from the Agency for Healthcare Research and Quality
References
Bacon, C.T., Trent, P., McCoy, T.P. (2018). Enhancing systems thinking for undergraduate nursing students using Friday night at the ER. Journal of Nursing Education, 57(11), 687-689. https://doi.org/10.3928/01484834-20181022-11
Clark, K., & Hoffman, A. (2019). Educating healthcare students: Strategies to teach systems thinking to prepare new healthcare graduates. Journal of Professional Nursing, 35(3), 195-200. https://doi.org/10.1016/j.profnurs.2018.12.006
Dolansky, M.A, & Moore, S.M. (2013). Quality and safety education for nurses (QSEN): The key is systems thinking. The Online Journal of Issues in Nursing, 18(3). https://doi.org/10.3912/OJIN.Vol18No03Man01
Dolansky, M. A., Moore, S. M., Palmieri, P. A., & Singh, M. K. (2020). Development and Validation of the Systems Thinking Scale. Journal of general internal medicine, 35(8), 2314-2320. https://doi.org/10.1007/s11606-020-05830-1
Phillips, J.M., & Stalter, A.M. (2016). Integrating systems thinking into nursing education. The Journal of Continuing Education in Nursing, 47(9), 395-397. https://doi.org/10.3928/00220124-20160817-05
Phillips, J.M., Stalter, A.M., Dolansky, M.A., & McKee-Lopez, G. (2016). Fostering future leadership in quality and safety in health care through systems thinking. Journal of Professional Nursing, 32(1), 15-24. https://doi.org/10.1016/j.profnurs.2015.06.003
Plack, M. M., Goldman, E. F., Scott, A. R., & Brundage, S. B. (2019). Systems thinking in the healthcare professions: A guide for educators and clinicians. Washington, DC: The George Washington University.